Live
- Jhansi meets people during her morning walk
- World Liver Day 2024: Theme, History, and Significance
- Google Pixel 9 Rumoured AI Features: Magic Composer, Autofill Smart Reply, and More
- Malladi Vishnu complains to EC on Naidu, Ayyanna & Pawan
- MyVoice: Views of our readers 19th April 2024
- Peddireddi touched my feet for DCC post, recalls Kiran
- All politicos must commit to free press
- iPhone 17 Plus Rumors: Potential Smaller Screen Size for the 2025 iPhone
- Risk of Middle East escalation
- 50 families quit YSRCP, join TDP
Just In
All deaths are tragic, but some are sadder than usual. For instance a person, who is unwell, seeks intervention, is denied vital help, and dies a hapless death.
All deaths are tragic, but some are sadder than usual. For instance a person, who is unwell, seeks intervention, is denied vital help, and dies a hapless death.
Most unfortunate are those who lose their chance at life like this, because someone is afraid to stretch out a helping hand.
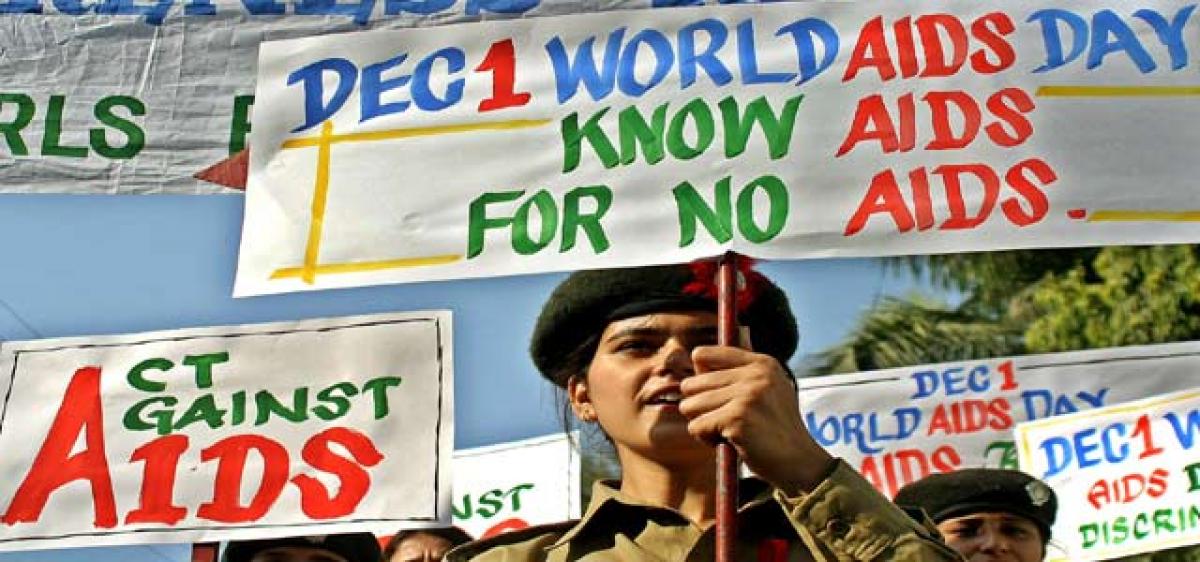
As HIV/AIDS programmes in India touch the two-decade mark, the agencies involved in their implementation have many gains to count but still struggle with some crucial inadequacies in terms of resources, policy, support mechanisms and social awareness.
The National AIDS Control Programme IV, which ends in a few months, while continuing to focus on prevention with Targeted Interventions and scaling up of testing facilities, blood transfusion facilities and a new protocol for PPTCT, sharply emphasises on substantial treatment facilities for People Living with HIV/AIDS.
However, changes like the withdrawal of international donors from the bulk of the interventions and essential operational responsibilities shifted from implementing partners to civil society organisations, have affected its sustainability. Treatment takes a direct hit with people already on Anti-Retroviral Therapy (ART) left high and dry as necessary support services dwindled across the last few years.
Even as treatment facilities scale up, necessary support mechanisms are lacking, say those on Anti-Retroviral Therapy (ART). Ahead of the World AIDS Day, which is on December 1, we analyse the HIV/AIDS programmes in India, which touch the two-decade mark this year. Despite many achievements they lack crucial resources, policy support mechanisms and most of all, social awareness
The Telangana State AIDS Control Society, whose entire funding is received from the Centre, continues to coordinate treatment facilities with drug supply from the Global Fund to fight AIDS, Tuberculosis and Malaria, combined with National AIDS Control organisation and Union government funding.
Treatment facilities, as a matter of fact, have been scaled up substantially. While the first batch of patients administered the ART was a mere 200 at the Osmania Hospital back in 2004, the number has gone up multifold with more than 4,000 PLHAs now receiving ART there.
As of October 2016, a total of 1.7 lakh PLHAs, including those on pre-ART, are registered for the ART in Telangana, with 22 centres offering treatment across the State.
Out of the 86,548 PLHA under active care, 63,624 PLHA are on ART. Out of 8,323 children registered at the ART Centres, 2,786 are already receiving treatment.
Even as treatment facilities are getting scaled up, necessary support mechanisms are totally lacking, say those on ART.
Treatment management support from the State government is far from satisfactory in terms of psychological counselling facilities, management of opportunistic infections, and side effects of toxic drugs.
As the harsh drug regimen takes a heavy toll on the patient’s general well-being and drug fatigue sets in, the PLHA need supportive care with nutrition counselling, psychological support and timely treatment for opportunistic infections, such as tuberculosis, skin infections, gynaec problems, ulcers, etc.
“I was the first person to receive Stavudine drug in the State and have completed a negative effect-free five years.
It was a successful experiment of sorts but then I am on Zidovudine for six years now but, there is no review or assessment to check whether I need a drug change,” explains Priya, Founder of Cheyutha and Women CBO working on HIV/AIDS, and one of the first ever PLHAs in the State to stand for the rights of the community.
The absence of supportive care for those affected by long-term drug use has led to many Lost to Follow-up cases with people giving up drugs and vanishing, leading to deterioration in their health and hence quick death.
“Adherence is the key in ART and due to negligence in follow-up, deaths among PLHA are going up,” admits a senior official from the TSACS.
“However, we find that children on ART, especially those under institutional care are doing much better. This makes a case for proper nutrition, psychological care and supportive care,” the official says.
A cardiac surgeon once told me ‘the needles are too small and sharp, madam. I can’t risk my life.’ How many times can we fight this discrimination?” asks Priya, Founder of Cheyutha and Women CBO
Medical discrimination
While ART centres are themselves not designed to offer anything beyond the core therapy and Support Centres being withdrawn as the HIV/AIDS programme progressed, another factor that really hits the entire treatment strategy hard is medical discrimination.
“We were once sitting in an Arogyasri meeting at NIMS Hospital, Hyderabad, where the doctor concerned claimed that no PLHA cases were sent there.
But, I personally know cases where PLHA with diabetes, TB, liver damage and cardiac issues have been turned away once it was established that the patient was HIV Positive,” Priya reveals.
“The doctors cite reasons like shortage of disposables and drugs, lack of equipment and personnel, even that the patient is not a fit candidate for surgery, when a PLHA needs one.
We had a case of a woman, a State gazette officer due for a promotion, dying because she could not get timely treatment,” she informs.
While births and hysterectomies are still carried out without much difficulty, other surgeries like cardiac, angiograms, piles and hernia, eye and ear procedures are still not done by doctors that are too nervous to handle Positive patients.
“A cardiac surgeon once told me ‘the needles are too small and sharp, madam. I can’t risk my life.’ How many times can we fight this discrimination?” asks Priya.
“It is difficult to keep track of people with infections, those who are discriminated against and the ones dying,” she laments.
“Yes, we do know that discrimination exists, not just socially but also among the medical community. We will certainly address it.
We plan to launch a dialogue again,” asserts Karuna Vakati, Commissioner, Health and Family Welfare, who holds the additional charge as Project Director, TSACS, the second official to hold an additional charge while TSACS undoubtedly needs a full-time PD.
“Some of the government hospitals are even carrying out HIV tests without proper consent from the patient. Law says that there should at least be necessary consent from the attendant but hospitals carry out HIV tests as a matter of routine. Repeated reminders from us are ignored,” alleges the TSACS official.
However, doctors from these hospitals and NIMS deny the said allegations, saying that there is no discrimination at all.
“We have many people getting surgeries done here and as far as the testing is concerned, when a surgery is essential, these tests are mandatory.
It is after all our lookout to ensure safe surgeries,” says a senior doctor from NIMS, who wants to remain anonymous.
No emphasis on awareness
“The programme has come unhinged in the recent years. We no longer have the same support from the government as we did years back.
There is no funding, except for a couple of organisations and that too on just a few components. HIV/AIDS was hyped up when it was a major issue internationally. Now we are a forgotten community,” a representative of PLHA Network is sorrowful.
“There is no emphasis now on awareness whereas there is a new batch of doctors every now and then.
We need to go on orienting the doctors to the fact that there are safeguards against risk in operating upon PLHV.
As we still need to do with teachers and community leaders to ensure a discrimination-free society,” Priya says.
Lack of financial support is another issue that makes sustenance difficult for an already beleaguered community.
Cheyutha, for instance, runs with support from Value Labs, ADP Ltd, Lepra, Indian Red Cross Society and Joy group of the 1992 class of St Marks School, of which Priya is also an alumnus.
One of the primary objectives of the Avahan Project, funded by the BMGF, was to hand over the HIV/AIDS programme to Community-based organisations and NGOs after certain years and the programme focuses on transition in its sunset years.
Yet, the CBOs are struggling to survive. “Small organisations such as ours do not get any institutional support. We operate like a Self-help group and rotate our own individual donations.
This forces us to go back to the profession of sex work whether or not we like it,” says Vijaya Lakshmi of the Suryodaya Kiranam Mahila Sangham, a CBO of positive sex workers.
“We are a welfare state and I believe the government should address the problems of PLHA as a matter of priority. It will be done,” assures Karuna Vakati.
People Living with HIV/AIDS are among the most vulnerable in society. Not just because of their physical health but also due to their social and economic status; and due to continuing stigma and discrimination.
Medicine and food, care and support, advice and guidance are the very minimum that the State and society can offer to keep their spirits high - to simply keep them alive.

© 2024 Hyderabad Media House Limited/The Hans India. All rights reserved. Powered by hocalwire.com







