Live
- Four power plants hit in massive Russian overnight attacks on Ukraine
- International Marconi Day 2024 Date, history and significance
- Congress slits throat of Hindu people for Muslims, alleges Giriraj Singh
- Anupama Parameswaran Goes De-Glam for Powerful New Film ‘Paradha’
- Members of Erukal community in Dharmavaram join BJP ahead of elections
- MLA Candidate Visits Gyms in Visakha North Constituency, Promises Development If Elected"
- Yes Bank net profit doubles to Rs 452 crore in Jan-March quarter
- Has Allu Arjun Set his Fee at Rs 150 Crore for 'Pushpa 2'?
- Early detection of 'osteoarthritis' may allow therapy that improves joint health: Researchers
- ‘Prasanna Vadanam’ Trailer: Suhas Starrer Promises a Unique Rom-Com Thrill Ride
Just In
The Silent Epidemic of Antimicrobial Resistance: A Quintuple Whammy

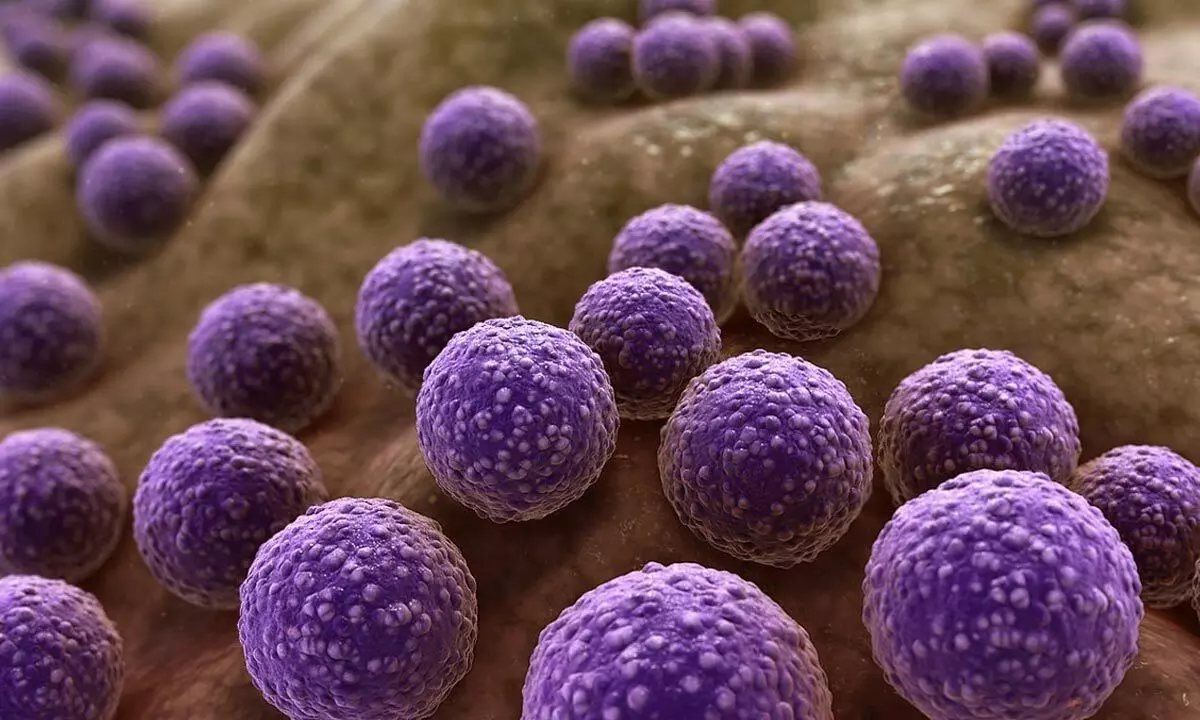
Antimicrobial resistance (AMR) is an imminent threat to global public health, contemporary health systems, and economies
Antimicrobial resistance (AMR) is an imminent threat to global public health, contemporary health systems, and economies. When microbes evolve resistance to lifesaving drugs, the burden presents a powerful quintuple whammy that policy experts must recognize and respond to.
(1) Antibiotics becoming ineffective
The misuse and overuse in humans, animals, and plants have rendered antibiotics ineffective. A report by Lancet states that AMR was directly responsible for at least 1.27 million deaths and indirectly associated with nearly five million deaths globally in 2019. The burden of fatalities is disproportionately more on low- and middle-income countries (LMICs). Besides mortality, the potential impacts of rising AMR include fewer effective treatment options, higher morbidity, more costly treatments, and higher loss of person days from work. Uncertainties over the growth path of AMR over time, the functional relationship between antibiotic use and AMR, and morbidity/mortality directly attributable to AMR (in contrast to other underlying causes) make this issue furthermore contentious.
(2) Stagnant discovery
Although the discovery of novel antibiotics peaked between the 1950s and the 1970s, it has stagnated since the 1980s. The antibiotics brought to the market in the past three decades are modifications of previously discovered drugs. These are inadequate to serve the growing unmet requirements and resistance.
(3) Limited access
The LMICs have limited access to new and effective antibiotics that are variants of existing classes. For instance, the global antibiotics consumption rate between 2000 and 2018 has shot up 46 percent, from 9.8 to 14.3 defined daily doses (DDD) per 1000 population per day. In contrast, the variation between countries in consumption rates has risen ten-fold, ranging from as low as 5 DDD to 45.9 DDD per 1000 population per day. As per a study published in the Clinical Infectious Diseases Journal, 11 out of 14 countries have access to less than half of eighteen new antibacterials developed between 2010-19.
(4) Market Failure
A significant problem is the ‘far-from-perfect’ antibiotic market. The conditions encouraging or extenuating the development and spread of AMR are driven by choices made by veterinarians and farmers, doctors and patients, industry and governments, etc., concerning what antibiotics to produce, purchase, and use. Choices, in turn, are determined by the markets that reinforce whether, what, and how much – a producer may invest in antibiotics production and the price that the consumer will pay. However, the market for antibiotics is heavily affected by two forces. First, the ‘public good’ attributes of antibiotics affect consumption and distribution, resulting in less than socially optimal levels of either antibiotic consumption or production. Second, there are negative externalities arising from antibiotic consumption, such as adverse external effects on future patients who may require antibiotics and broadly on the health care systems that are not included in the decision to consume. In either of these two cases, left on its own, the markets will ‘fail’ and not result in socially optimum outcomes. This will not only dilute economic efficiency but also incapacitate distributional justice in terms of access to antibiotics and the impact of AMR.
(5) Mass Exodus from R&D space
It is also intriguing that the pharma players engaged in anti-bacterial agent development are predominately small firms with nearly 80 percent share in the new antibiotic discoveries globally. In contrast, large firms and non-profit institutes/universities hold minuscule shares of 12 percent and 08 percent, respectively. Many large pharmaceutical companies have discontinued antibiotic research and development (R&D). One argument peddled by large companies is that the cost-benefit ratio of antibiotic development is economically unfavorable compared to other profitable drugs. In addition, antibiotics are inexpensive, sell in a lower volume, and are unpredictable due to the sporadic nature of infections and outbreaks. So, under the guise of high-risk, low-return proposition in antibiotic development, big pharma companies continue to rack up profits through other drugs. A study by the Centre for Science and Environment (CSE) finds that 11 of the world’s 15 big pharma companies do not have antibiotics in their pipeline. Only 13 out of the 1007 molecules in the clinical pipeline of these 15 giant companies are antibacterial agents. This contrasts sharply with 411 agents developed for cancer, 150 for immunology, allergy, inflammation, or respiratory diseases, and 84 for cardiology, metabolism, or renal disease areas. Going by the same high-risk, low-return proposition, it is just a matter of time before small companies will face diminishing values and eventually pull out in trying to pick up the slack.
Fixing the Market: The Way Forward
A combination of ‘push’ and ‘pull’ incentives is required to overcome market failure and create a robust antibiotic R&D ecosystem. The push incentive, such as support in innovation and R&D funds for new antibiotics regardless of success in market access, will tend to reduce the developers’ costs and risks through financial, tax, and technical inducements. An example could be funders' pooling and sharing of failure risks, including governments and private firms. On the other hand, the pull incentive, such as rewards for new, scientifically viable, and market-relevant antibiotics, will reduce the risk of insufficient future revenues by utilizing mechanisms and ensuring developers’ financial viability. While the governments will have to play a more significant role, their efforts must be supplemented by adequate private-sector participation, especially in LMICs. Moreover, it is critical to consider all costs and benefits of antimicrobial use, including those arising from externalities, to inform policymakers on strategies to contain the impact of AMR.
To conclude, antibiotics are a ‘global’ public good. Their preservation and development for future generations through ‘sustainable and equitable access’ should be at the forefront of public policy-making to avert a dire health emergency.
***
The author is an Associate Professor of Economics at the Kalinga Institute of Industrial Technology (KIIT) Deemed University, Bhubaneswar. Email: saswat.mishrafcm@kiit.ac.in. Views are personal.

© 2024 Hyderabad Media House Limited/The Hans India. All rights reserved. Powered by hocalwire.com






