Live
- PIL in SC seeks direction to designate BMC as sole planning, sanctioning authority for Mumbai
- 3rd Test: Centuries from Head, Smith help dominant Australia feast on listless India
- AAP final list of 38 names in Delhi: Kejriwal, CM Atishi retain seats
- Tributes Paid to Sardar Vallabhbhai Patel on His Death Anniversary at CM Revanth Reddy's Residence
- In just one year, Bhajanlal govt wins hearts of people
- CM Chandrababu announces establishment of Potti Sriramulu Telugu University
- Sutume, Kissa win World 25K Kolkata; India's Gulveer makes course record
- US accounts for 18 per cent of Indian exports in FY24
- Will end Naxalism in Chhattisgarh by March 2026: Amit Shah
- Will gift one project daily to people during Jan Kalyan Parv
Just In
Globalisation and improved transportation has made the diseases more contagious. The year 2015-16 has witnessed breakout of most contagious diseases like Ebola, Swine Flu and Zika, hence a question is expected in the prelims as well as mains.
Human civilisation has advanced many folds since its inception; technological advances have solved most deadly diseases like cholera, tuberculosis, rabies, brain fever and polio. But as years pass by new deadly diseases are killing population more than before.
Globalisation and improved transportation has made the diseases more contagious. The year 2015-16 has witnessed breakout of most contagious diseases like Ebola, Swine Flu and Zika, hence a question is expected in the prelims as well as mains.
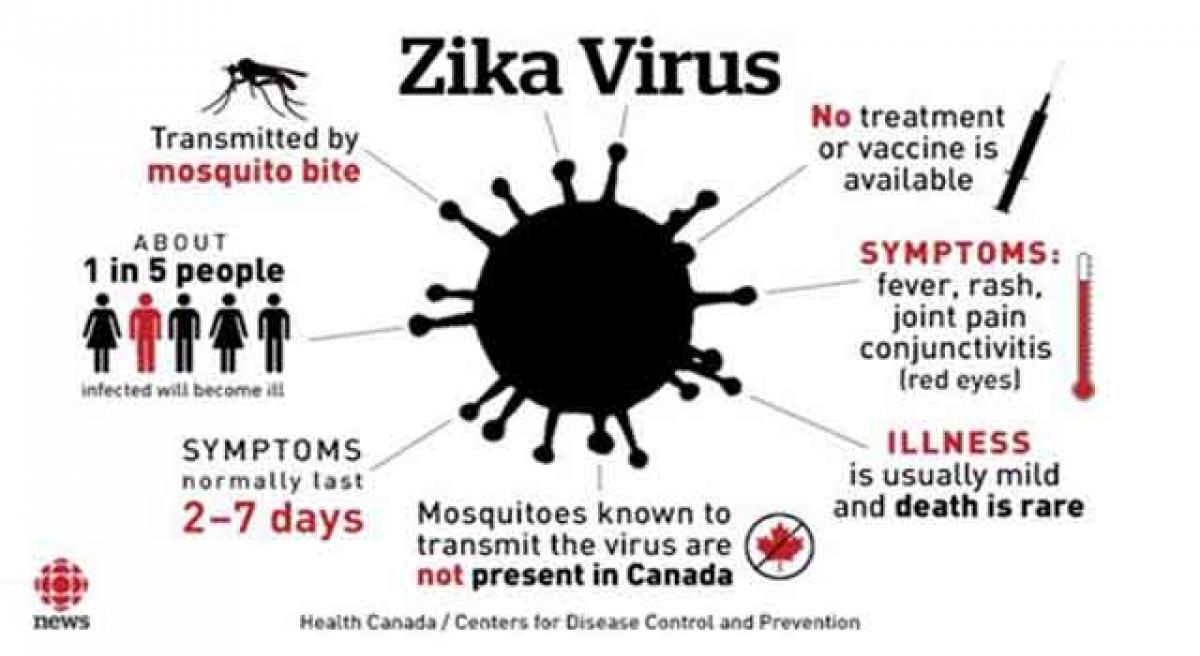
Zika Virus
Zika virus is a mosquito-borne flavivirus that was first identified in Uganda in 1947 in monkeys through a network that monitored yellow fever. It was later identified in humans in 1952 in Uganda and the United Republic of Tanzania. Outbreaks of Zika virus disease have been recorded in Africa, the Americas, Asia and the Pacific.
From the 1960s to 1980s, human infections were found across Africa and Asia, typically accompanied by mild illness. The first large outbreak of disease caused by Zika infection was reported from the Island of Yap (Federated States of Micronesia) in 2007. In July 2015 Brazil reported an association between Zika virus infection and Guillain-Barré syndrome. In October 2015 Brazil reported an association between Zika virus infection and microcephaly.
Signs and Symptoms
The incubation period (the time from exposure to symptoms) of Zika virus disease is not clear, but is likely to be a few days. The symptoms are similar to other arbovirus infections such as dengue, and include fever, skin rashes, conjunctivitis, muscle and joint pain, malaise, and headache. These symptoms are usually mild and last for 2-7 days.
Complications of Zika virus disease
After a comprehensive review of evidence, there is scientific consensus that Zika virus is a cause of microcephaly and Guillain-Barré syndrome. Intense efforts are continuing to investigate the link between Zika virus and a range of neurological disorders, within a rigorous research framework.
Transmission
Zika virus is primarily transmitted to people through the bite of an infected mosquito from the Aedes genus, mainly Aedes aegypti in tropical regions. Aedes mosquitoes usually bite during the day, peaking during early morning and late afternoon/evening. This is the same mosquito that transmits dengue, chikungunya and yellow fever. Sexual transmission of Zika virus is also possible. Other modes of transmission such as blood transfusion are being investigated.
Treatment
Zika virus disease is usually mild and requires no specific treatment. People sick with Zika virus should get plenty of rest, drink enough fluids, and treat pain and fever with common medicines. If symptoms worsen, they should seek medical care and advice. There is currently no vaccine available.
Key facts
- Zika virus disease is caused by a virus transmitted primarily by Aedesmosquitoes.
- People with Zika virus disease can have symptoms including mild fever, skin rash, conjunctivitis, muscle and joint pain, malaise or headache. These symptoms normally last for 2-7 days.
- There is scientific consensus that Zika virus is a cause of microcephaly and Guillain-Barré syndrome. Links to other neurological complications are also being investigated
Mission Indradhanush
Mission Indradhanush was launched by the Ministry of Health and Family Welfare, Government of India on December 25, 2014. Between 2009-2013 immunization coverage has increased from 61% to 65%, indicating only 1% increase in coverage every year. To accelerate the process of immunization by covering 5% and more children every year, Indradhanush mission has been adopted to achieve target of full coverage by 2020.
Objective
The Mission Indradhanush, depicting seven colours of the rainbow, aims to cover all those children by 2020 who are either unvaccinated, or are partially vaccinated against seven vaccine preventable diseases which include
1.diphtheria,
2.whooping cough,
3.tetanus,
4.polio,
5.tuberculosis,
6.measles and
7.hepatitis B
Areas Under Focus
Mission Indradhanush will target 201 high priority districts in the first phase and 297 districts for the second phase in the year 2015. During the first phase, 201 high focus districts in the country which have nearly 50% of all unvaccinated or partially vaccinated children would be covered.
Out of the 201 districts, 82 districts are in just four states of UP, Bihar, Madhya Pradesh and Rajasthan. Nearly 25% of the unvaccinated or partially vaccinated children of India are in these 82 districts of 4 states.
Within the districts, the Mission will focus on the 400,000 high risk settlements identified by the polio eradication programme. These are the pockets with low coverage due to geographic, demographic, ethnic and other operational challenges. Evidence has shown that most of the unvaccinated and partially vaccinated children are concentrated in these areas.
The following areas will be targeted through special immunization campaigns:
1.High risk areas identified by the polio eradication programme. These include populations living in areas such as:
- Urban slums with migration
- Nomads
- Brick kilns
- Construction sites
- Other migrants (fisherman villages, riverine areas with shifting populations etc.) and
- Underserved and hard to reach populations (forested and tribal populations etc.)
2.Areas with low routine immunization (RI) coverage (pockets with Measles/vaccine preventable disease (VPD) outbreaks).
3.Areas with vacant sub-centers: No ANM posted for more than three months.
4.Areas with missed Routine Immunisation (RI) sessions: ANMs on long leave and similar reasons
5.Small villages, hamlets, dhanis or purbas clubbed with another village for RI sessions and not having independent RI sessions.
Swine Flu
Swine flu is a highly contagious respiratory disease in pigs caused by one of several swine influenza A viruses. Transmission of swine influenza viruses to humans is uncommon. However, the swine influenza virus can be transmitted to humans via contact with infected pigs or environments contaminated with swine influenza viruses.
Swine Flu Symptoms
These, too, are pretty much the same as seasonal flu. They can include:
- Cough
- Fever
- Sore throat
- Stuffy or runny nose
- Body aches
- Headache
- Chills
- Fatigue
Like the regular flu, swine flu can lead to more serious problems including pneumonia, a lung infection, and other breathing problems. And it can make an illness like diabetes or asthma worse
Spread of flu
The H1N1 virus is spread in exactly the same way as the common cold and other flu viruses.
The virus is contained in the millions of tiny droplets that come out of the nose and mouth when someone coughs or sneezes.
These droplets typically spread about 1 metre (3 feet). They hang suspended in the air for a while, but then land on surfaces, where the virus can survive for up to 24 hours.
Anyone who touches these surfaces can spread the virus by touching anything else. The virus is also transmitted by infected people who cough or sneeze into their hands and then touch other people or objects before washing their hands.
Everyday items at home and in public places may have traces of the virus. These include food, door handles, remote controls, hand rails, paper money and computer keyboards.
People usually become infected by picking up the virus on their hands from contaminated objects and then placing their hands near their mouth or nose. It is also possible to breathe in the virus if it is suspended in airborne droplets.
People who are at increased risk for severe complications from influenza
- Children under 5 years old
- People 65 or older
- Children and teens (under age 18) who are getting long-term aspirin therapy and who might be at risk for Reye's syndrome after being infected with swine flu. Reye's syndrome is a life-threatening illness linked to aspirin use in children.
- Pregnant women
- Adults and children with chronic lung, heart, liver, blood, nervous system, neuromuscular, or metabolic problems
- Adults and children who have weakened immune systems (including those who take medications to suppress their immune systems or who have HIV)
- People in nursing homes and other long-term care facilities
What is the incubation period for swine flu?
The incubation period for swine flu is about one to four days, with the average being two days; in some people, the incubation period may be as long as about seven days in adults and children.
What is the contagious period for swine flu?
The contagious period for swine flu in adults usually begins one day before symptoms develop in an adult and it lasts about five to seven days after the person becomes sick. However, people with weakened immune systems and children may be contagious for a longer period of time (for example, about 10 to 14 days).
How long does the swine flu last?
In uncomplicated infections, swine flu typically begins to resolve after three to seven days, but the malaise and cough can persist two weeks or more in some patients. Severe swine flu may require hospitalization that increases the length of time of infection to about nine to 10 days
What is the treatment for swine flu?
The best treatment for influenza infections in humans is prevention by vaccination. Work by several laboratories has produced vaccines. The first H1N1 vaccine released in early October 2009 was a nasal spray vaccine that was approved for use in healthy individuals ages 2-49.
The injectable vaccine, made from killed H1N1, became available in the second week of Oct. 2009. This vaccine was approved for use in ages 6 months to the elderly, including pregnant females. Both of these vaccines were approved by the CDC only after they had conducted clinical trials to prove that the vaccines were safe and effective. A new influenza vaccine preparation is the intradermal (trivalent) vaccine is available; it works like the shot except the administration is less painful. It is approved for ages 18-64 years.
Implementation of mission indradhanush
Focused and systematic immunization drive will be through a “catch-up” campaign mode where the aim is to cover all the children who have been left out or missed out for immunization. Mission Indradhanush Phase I was started as a weeklong special intensified immunization drive from 7th April 2015 in 201 high focus districts for four consecutive months.
During this phase, more than 75 lakh children were vaccinated of which 20 lakh children were fully vaccinated and more than 20 lakh pregnant women received tetanus toxoid vaccine. Government has launched Phase II of Mission Indradhanush in selected 352 districts in the country of which 279 are medium focus districts and remaining 73 are high focus districts of Phase-I.
During Phase II of Mission Indradhanush, four special drives of weeklong duration are being conducted starting from October 2015. The Ministry will be technically supported by WHO, UNICEF, Rotary International and other donor partners. Mass media, interpersonal communication, and sturdy mechanisms of monitoring and evaluating the scheme are crucial components of Mission Indradhanush.
By:Balalatha Mallavarapu

© 2024 Hyderabad Media House Limited/The Hans India. All rights reserved. Powered by hocalwire.com







