Cervical cancer and the human papilloma virus vaccination
Cervical cancer remains the most common gynaecological cancer and the third most common malignancy in women worldwide. Highest incidences tend to occur in populations with low screening rates combined with a high background prevalence of human papilloma virus (HPV) infection and liberal attitudes towards sexual behaviour
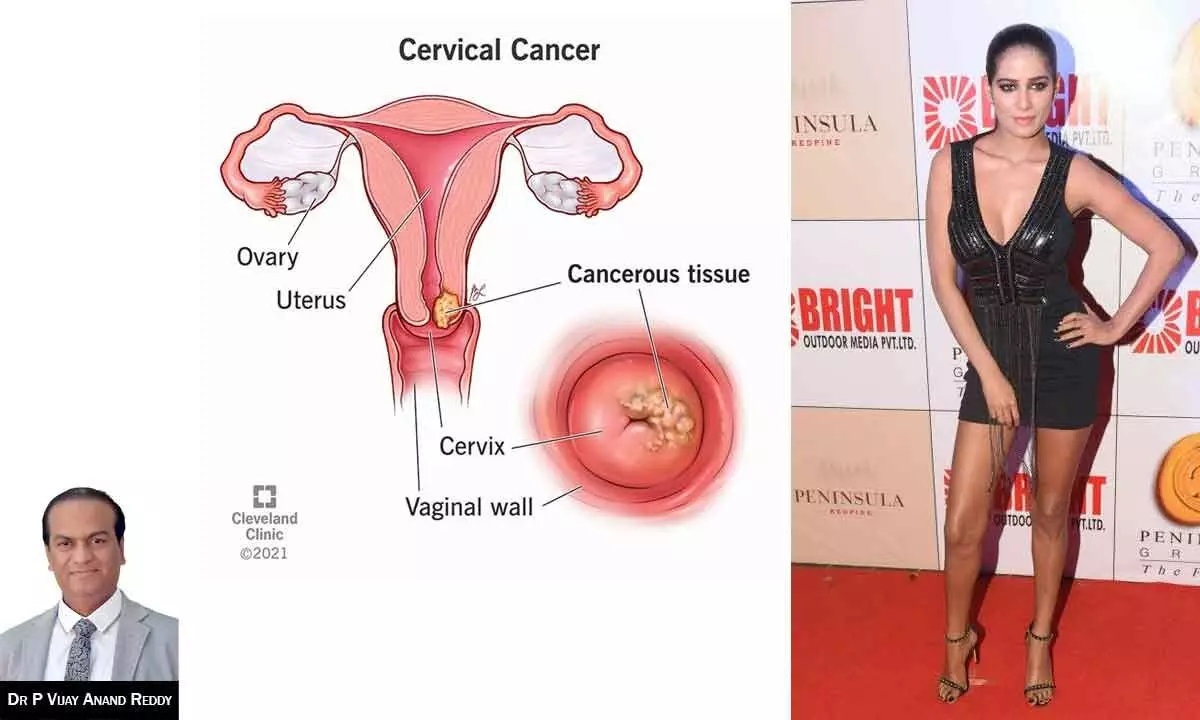
Poonam Pandey, the famed Indian model and actress, shocked her fans and the nation when she revealed her battle with cervical cancer. Despite her glamorous image on-screen, Poonam’s diagnosis highlighted the indiscriminate nature of this disease.
Cervical cancer, as detailed in medical literature, remains a significant health concern globally, affecting women of all backgrounds. The prevalence of this malignancy underscores the importance of awareness, prevention, and early detection measures.
Poonam’s journey with cervical cancer shed light on the crucial role of human papillomavirus (HPV) vaccination in preventing this disease. While her story served as a reminder of the importance of routine screening and vaccination, it also emphasized the need for comprehensive healthcare access for all individuals, regardless of their social status or celebrity status.
Despite the challenges posed by her diagnosis, Poonam Pandey’s public battle with cervical cancer sparked conversations about women’s health and encouraged many to prioritize their well-being through preventive measures and regular screenings.
Cervical cancer remains the most common gynaecological cancer and the third most common malignancy in women worldwide. Highest incidences tend to occur in populations with low screening rates combined with a high background prevalence of human papilloma virus (HPV) infection and liberal attitudes towards sexual behaviour.
The risk factors associated with increased predisposition for cervical cancer includes initiation of sexual intercourse at young age, multiple sexual partners, promiscuous sexual behaviour in male partners, low socio-economic status, poor access to health care, high parity, smoking, presence of infections such as HPV, HIV.
Dr P Vijay Anand Reddy, MD, DNB, Director, Apollo Cancer Centre, Apollo Hospitals, Hyderabad says, “Human papilloma virus (HPV) is a double stranded DNA virus, that can be easily spread through direct sexual contact, from the skin and mucous membranes of the infected people. Sexually transmitted HPV types fall into either low risk or high-risk categories. Low risk HPV (6,11) do not cause cancer, while the high-risk subtypes 16 and 18 cause cancer. It is estimated that more than 90% of cervical cancers ae related to the presence of HPV and is now accepted as a necessary cause of most cervical cancers.”
Although there is high prevalence of HPV worldwide, peaking at ages 25 to 35 years, less than 15% of the exposed women develop persistent infection that results in dysplasia. Most of the women clear the infection within 2 years.
Screening: Regular screening of women between the ages of 21 and 65 years with Pap smear test decreases their chance of dying from cervical cancer. Women less than 21 years of age should not be screened regardless of the age at sexual initiation. Upto the age of 65 years, cytology should be performed every 3 years. When both the HPV test and Pap test are done using cells from the sample removed during a Pap test, it is called a Pap/HPV co-test. HPV Co-test is not recommended in women less than 30 years of age. In those above 30 years, HPV co-test is to be performed as a routine screening procedure every 5 years. HPV DNA test may be used without a Pap test for cervical cancer screening in women aged 25 years and older every 3 years.
Prevention: Vaccination against human papillomavirus (HPV) has had a significant impact on reducing the incidence of cervical cancer. HPV vaccines, such as Gardasil and Cervarix, target high-risk HPV types associated with the development of cervical cancer. By vaccinating individuals before they become sexually active, the vaccines effectively prevent infection with these high-risk HPV types, providing long-term protection. This, in turn, lowers the risk of cervical cancer and its precursor lesions. Various research trials showed that HPV vaccination provides 99% protection against cervical cancer.
Two types of vaccines are available to prevent the human papillomavirus (HPV) types that cause most cervical cancers. Quadrivalent vaccine (HPV 6,11,16,18) and Bivalent vaccine (HPV 16,18) are the two FDA approved vaccines against HPV. The Quadrivalent vaccine is given as 3 doses at 0, 2 and 6 months while the Bivalent vaccine is given as 3 doses at 0, 1 and 6 months.
HPV vaccination is recommended for 9- to 26-year-old females. Ideally females should get the vaccine before they become sexually active and exposed to HPV. Females who are sexually active may also benefit from vaccination, but they may get less benefit. This is because they may have already been exposed to one or more of the HPV types targeted by the vaccines. However, few sexually active young women are infected with all HPV types prevented by the vaccines, so most young women could still get protection by getting vaccinated. However, it is important that women continue to be screened for cervical cancer, even after getting all 3 doses of either HPV vaccine. This is because neither vaccine protects against all types of cervical cancer. HPV vaccination is not currently recommended for women over age 26 years. The best way to prevent cervical cancer is to get routine cervical cancer screening, as recommended.
Indian government has implemented various initiatives to promote HPV vaccination and combat cervical cancer. The government has integrated the HPV vaccine into its immunization programs, particularly for adolescent girls free of cost.
Treatment and Outcome
Cervical cancer is highly curable cancer. Stage 1 cancer can be treated either with surgery or radiation. Stage 2 -3 cervical cancer can be treated with Chemoradiation therapy. In a stage 4 cancer patient needs chemotherapy. It is a highly curable cancer with 5 yr survival rates as good as 90-95% in stage 1, 70-85% in stage 2, 60-70 % in stage 3 and 25% in stage 4.
As it is an easily detectable cancer by simple screening methods, it is imperative to implement screening programme for cervical cancer across the country.