Your Facial Pain might be A Trigeminal Neuralgia
TN is one of the most common causes of less productivity and low confidence levels causing severe disability in the work environment that leads to anxiety and depression in patients' lives
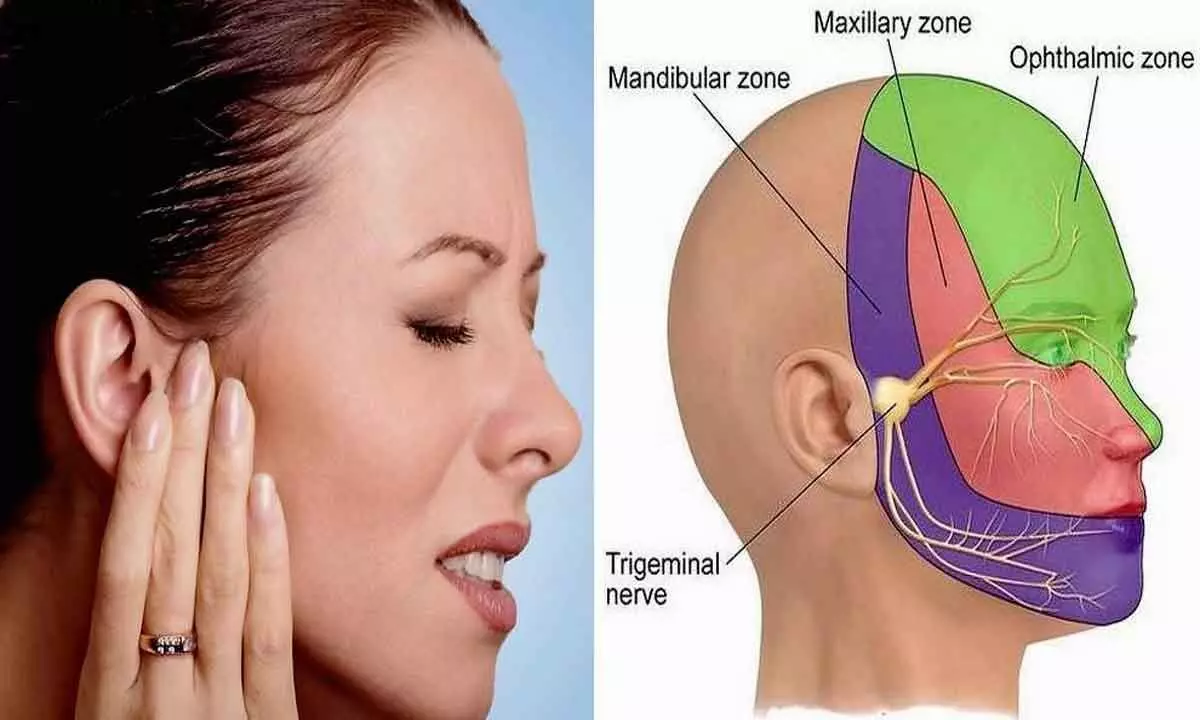
Trigeminal neuralgia (TN) refers to severe, sharp, recurrent, lancinating, electric shock-like facial pain that occurs in the distribution of one or more branches of the fifth cranial nerve over the face, cheeks and jaw. It lasts for a fraction of a second to almost 2 minutes. It is one of the commonest types of craniofacial pain disorders. The pain perception is typically unilateral, abrupt in onset, brief, and usually starts after trivial stimuli like touch, shaving and chewing food. Highly sensitive people can't tolerate cold air or air conditioner. Patients report that they can't speak or take food in its severe form. Most of the time, there is disturbed sleep and sudden arousal from sleep due to the pain present. Spontaneous pain ruins the focus of the work, and people notice pain during crucial activities like driving or conference meetings. TN is one of the most common causes of less productivity and low confidence levels causing severe disability in the work environment that leads to anxiety and depression in patients' lives.
The pain is most commonly felt in the distribution of the trigeminal nerve's maxillary (V2) or mandibular (V3) divisions, broadly categorised into two types: classical TN and TN due to other causes. When the cause of neuralgia is a demonstrated or presumed loop of an aberrant blood vessel, it is known as "Classical TN". Many other conditions can cause TN, like acute herpes, post-herpetic neuralgia, post-traumatic neuralgia, multiple sclerosis and space-occupying lesions, such as cerebellopontine angle tumour, arterio-venous malformation and meningioma. The overall incidence of TN is about 40–50 cases per one million, and the estimated prevalence is approximately 100–200 per million populations. Patients in the age range of 35–65 years are most commonly affected. TN is nearly twice more common in females than in males. Hereditary forms of TGN have been reported but are rare and constitute less than 4–5% of overall TGN. The pain associated with TN can be so severe and disabling that it is sometimes called the "suicide disease". Some old texts also refer to the disease as "prosopalgia", which is derived from two Greek words 'prosopon' (face) and 'algos' (pain). Severe bouts of TN can trigger repetitive facial muscle spasms that mimic facial tics, giving rise to the name "Tic Douloureux". "a painful affection of the face in sudden, sharp bouts, most commonly triggered by light touch or eating". TN is also sometimes called "Fothergill's disease". Several decades later, in the 1820s, Charles Bell localised this pain syndrome to the trigeminal nerve, after which the condition was known as "Trigeminal Neuralgia". Currently, carbamazepine or oxcarbazepine are the first-line medical drugs used for TN. Sweet and Wepsic first performed RF thermal lesioning of the trigeminal nerve in 1974. Retrogasserian gamma knife radiosurgery (GKRS) has become one of the mainstream methods of providing safe and efficacious treatment in patients with refractory lesions.
Great surgeon Walter E Dandy first time identified and reported that this pain is arising due to impingement of arterial and venous vascular loops on the trigeminal nerve. This was a landmark observation in the understanding of the pathophysiology of TN. The credit for further improvement of the surgical technique goes to Peter Jannetta with the advent of the operating microscope. He proved that anomalous vascular loops compressing the trigeminal nerve resulted in focal demyelination and alteration of neuronal physiology, leading to the pain of TN. After he publicised nearly 1200 cases in 1996, microvascular decompression (MVD) was established as the surgical treatment of choice in classical TN.
MVD surgery is the most effective method that offers a permanent solution for pain. With the advancement in surgery techniques and recent progress in microscopy and endoscopy, we can do surgery with a keyhole approach. In this surgery, we can separate the vessel from the nerve. We practice keeping a Teflon patch between the nerve and the vessel, which helps keep the vessel far away from the nerve. With time progresses, the refined surgical skills assist the patient in from recurrence. We can notice 10-15% recurrence in the literature at 10 years' time. So, 90% of patients get relief from this procedure. It is relatively safe and can be done without any complications.
Dr Laxminadh, the consultant neurosurgeon, performs this surgery regularly, and all patients reported instant pain relief and enjoyed pain-free life without any medications. This surgery is indicated in patients in severe pain despite taking one or two medications regularly. It is a very safe procedure with high-end cutting-edge technology, like neuronavigation, surgical microscope and endoscope; we can thoroughly observe the vascular loop or vessel compressing the nerve and separate it permanently.
Patients review
"My wife suffered from this pain for three years, and the medications she was prescribed gave high sedation that disturbed her the entire day and finally got rid of this pain with MVD surgery done by Dr Laxminadh now leading an excellent quality of life in her family and at professional front," says Ravi.
"My business meetings got spoiled with a painful condition and couldn't proceed with my presentation during that brief few seconds to a minute. It gave embarrassing moments, and MVD surgery done by Dr Laxminadh provided a permanent solution, and now I can participate in lengthy meets without any disturbance," says Thakkar.
(The doctor is an MBBS, MCh - Neuro Surgery, Consultant Neurosurgeon, Continental Hospitals, Hyderabad)
















